
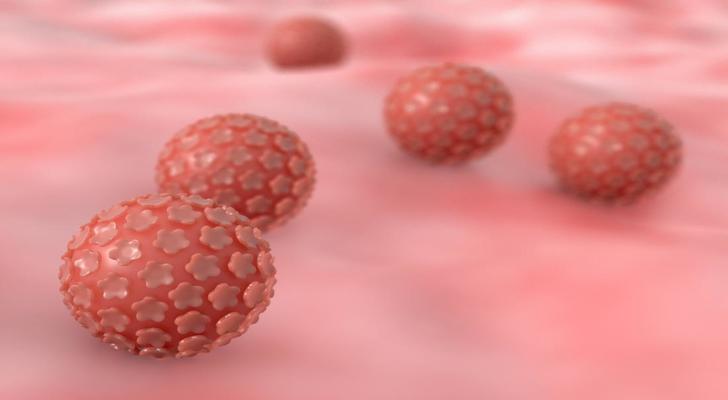
To begin with, it is useful to define Human Papillomavirus (HPV) in a medical context. HPV refers to a large group of related viruses transmitted primarily through skin-to-skin contact, including sexual contact. Infections occur in people of all sexes. There is no single universal test that detects every HPV infection; screening approaches exist for specific contexts. Many individuals have no symptoms and may be unaware of exposure.

Once the virus reaches the basal layers of the skin or mucosa through tiny abrasions or microtears, infection can occur. Transmission is commonly described with close skin-to-skin or intimate contact. Oral and genital sites can be involved, and the likelihood of transmission depends on the HPV type and the nature of contact, as outlined in clinical literature.
The symptoms of HPV are often subtle or absent. Many infections clear spontaneously within one to two years. Some HPV types are associated with anogenital or oral warts, while persistent infection with certain high-risk types is linked in research with cancers such as cervical cancer and a subset of other anogenital and oropharyngeal cancers. Descriptions emphasize variability in outcomes.

Multiple factors are discussed in association with higher likelihood of HPV acquisition or persistence. These include frequency of intimate contact, immunosuppression, disruptions of the skin or mucosal barrier, and direct contact with infectious lesions. Observational studies describe these contexts without assigning blame and note that risk differs by HPV type and site of infection.

Public health sources outline prevention themes in general terms. Examples commonly mentioned include vaccination programs for certain HPV types, use of barrier methods, and approaches aimed at reducing exposure to infectious lesions; for cutaneous (non-genital) warts, footwear in communal areas is sometimes discussed. These summaries are descriptive and not prescriptive.

How do clinicians describe HPV evaluation? Visible warts may be assessed by examination. In cervical cancer screening, methods include Pap tests and, in some settings, HPV testing to detect high-risk types. Application of dilute acetic acid (vinegar solution) is used in certain evaluations of suspected lesions. HPV DNA testing can further characterize types in appropriate clinical contexts, with sampling commonly obtained from the cervix.
Learn more about human papillomavirus (HPV) at Centers for Disease Control and Prevention.

