
Ischemic heart disease is a condition in which the heart muscle receives an inadequate blood supply. It is widely referred to as coronary artery disease. The process most often involves atherosclerotic plaque within coronary vessels, reducing the delivery of oxygen and nutrients required for cardiac function. When flow becomes sufficiently limited, areas of the myocardium may experience ischemia, and prolonged interruption can result in loss of viable tissue. Severe events include myocardial infarction.

Multiple factors are associated with this disease. Ischemic heart disease develops as plaque accumulates in coronary arteries, narrowing the vessel lumen. Reduced blood flow occurs when one or more arteries become partially or completely obstructed. Key coronary vessels that supply the heart include the left anterior descending, circumflex, and right coronary arteries, which deliver essential substrates to the myocardium. Their integrity is critical because these vessels nourish the heart.

Typical clinical features include angina, a discomfort often described as pressure, tightness, heaviness, or burning in the chest. Early recognition matters, as symptoms can emerge gradually or with exertion. Some individuals note radiation to the neck, back, jaw, or upper extremities. Heartburn can mimic chest discomfort, which occasionally leads to confusion about the source of pain. The overall pattern varies among people with ischemic heart disease.

Risk factors are frequently evaluated because they relate to disease likelihood and progression. Commonly cited factors include elevated blood pressure, increased LDL cholesterol, diabetes, higher body weight, limited physical activity, diets high in saturated fats, tobacco use, sleep disturbances, psychosocial stress, and certain pregnancy-related complications. Advancing age is associated with higher risk. These elements are considered collectively when assessing overall cardiovascular risk.
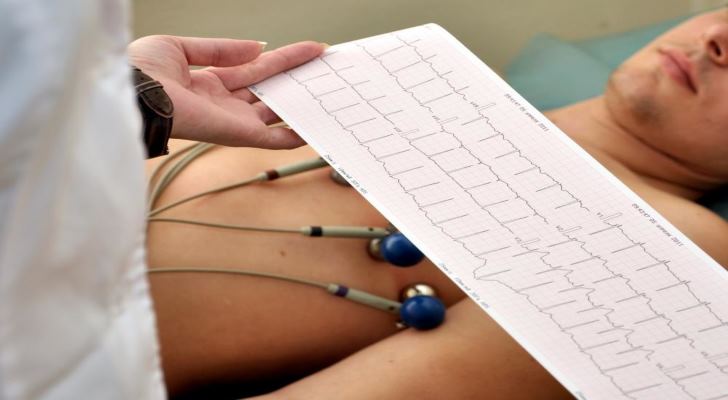
Diagnosis involves a combination of history, physical examination, and testing. An electrocardiogram (ECG) records cardiac electrical activity and can show rhythm and ischemic changes. Ambulatory monitoring, such as a Holter device, captures heart rhythms over time and compares them with expected ranges. Findings are interpreted in clinical context alongside other information from the evaluation.

Additional assessments may include echocardiography to evaluate chamber size, wall motion, and pumping function, as well as stress testing to observe performance under increased demand. In some settings, contrast dye is introduced to visualize coronary arteries during angiography. Computed tomography can provide information about coronary calcium and plaque burden. These imaging approaches help characterize anatomy and the extent of atherosclerotic change.

Questions often arise about whether risk can be modified. Research describes associations between modifiable factors and ischemic heart disease outcomes. Patterns of daily movement, body weight, lipid levels, blood pressure, and exposure to tobacco smoke are frequently discussed in relation to long-term cardiovascular health. Observational data highlight links between these parameters and disease trajectories.

Tobacco use and high alcohol intake are consistently associated with atherosclerosis and adverse cardiac events in population studies. Clinical assessments commonly include measurements of blood pressure and heart rate as part of routine cardiovascular evaluation. These observations are used to understand individual risk profiles rather than to prescribe specific actions within this overview.

Dietary patterns are also discussed in the literature. High sodium and saturated fat intake correlate with higher cardiovascular risk in many cohorts, while diets emphasizing fruits and vegetables correlate with more favorable risk profiles. Psychological stress is frequently examined for its associations with symptom patterns and cardiovascular outcomes. These relationships are descriptive and may vary by individual and study design.
Learn more about ischemic heart disease at Centers for Disease Control and Prevention.

