
A medical description of histoplasmosis is commonly phrased as a lung infection associated with inhalation of spores from the fungus Histoplasma capsulatum. The organism is unevenly distributed geographically, so exposure patterns differ by region. In many summaries, environmental reservoirs are linked to soil enriched by organic material. Sites inhabited by bats and areas frequented by birds are discussed as locations where droppings can accumulate and enrich soil with the fungus.

Infection can follow activities in areas where airborne spores are present. Many exposures are asymptomatic, and mild illness may resolve without specific intervention according to clinical overviews. More severe courses are described in people with reduced immune defenses or limited physiologic reserve. When dissemination occurs, involvement beyond the lungs has been documented, and cutaneous findings are reported in some immunocompromised individuals.
Soil disturbance in locations with accumulated organic material is frequently mentioned in relation to histoplasmosis. The infectious particles are microscopic spores that can become aerosolized in dust, which explains the absence of visible cues during exposure. Summaries also note roles for debris handling, demolition, or cleanup activities in dispersing contaminated dust into the air.

Re-exposures can occur in endemic regions. Prior infection may be followed by partial immunity in some people, yet subsequent illness remains possible. Environments with abundant organic enrichment of soil, including areas with accumulated bat or bird droppings, are repeatedly cited in environmental descriptions of exposure settings.
Symptoms, when present, are often nonspecific. Direct contact with droppings is not required, as inhalation of airborne spores is the usual route. Reported incubation intervals commonly range from about 3 to 17 days after exposure. Presentations may resemble influenza-like illness or pneumonia with fever and respiratory complaints, which can make distinction from other infections challenging based on initial features alone.

Described manifestations include chills, elevated temperature, chest discomfort, and a dry cough. Sweating can accompany fever. General malaise is frequently reported, and some accounts note joint pains. In more serious presentations, weight loss, shortness of breath, and marked fatigue are documented as part of systemic involvement.

Risk discussions indicate that anyone exposed in endemic areas may develop histoplasmosis, and repeated episodes are possible over a lifetime. Age patterns vary across reports, with young children and older adults appearing more often in some series. Immune status and preexisting lung disease are repeatedly highlighted as factors associated with more pronounced illness.

Occupational and avocational activities involving soil disruption or entry into sites with bat or bird droppings are described in case investigations. Examples in summaries include landscaping, demolition work, farming, and cleanup of enclosed spaces where organic material has accumulated.

Public health materials frequently frame prevention in terms of environmental exposure contexts. Narratives describe that exposure risk corresponds to activities that aerosolize contaminated dust in certain geographic areas. Descriptions focus on how location, type of activity, and disturbance of enriched soil can influence the likelihood of inhaling spores.

Environmental control discussions reference measures used in work settings to reduce dust generation during soil disturbance. Examples in technical summaries include wetting of surfaces and use of respiratory protection in specific occupational scenarios. These descriptions are presented in the context of workplace practices rather than individual medical guidance.

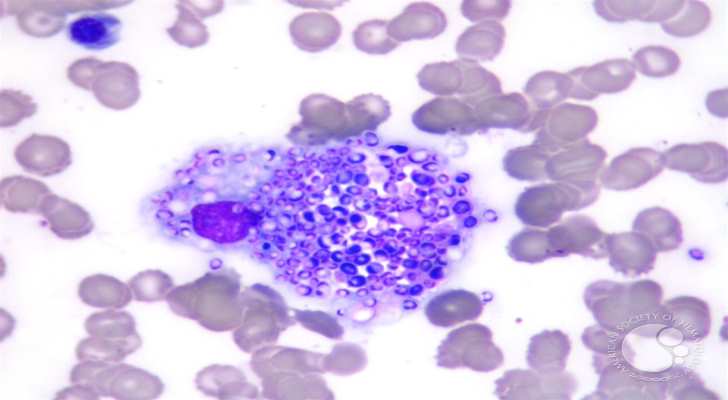
Diagnostic overviews note that many infections are subclinical. When evaluation is undertaken, commonly referenced tools include antigen detection assays in urine or blood, serology, cultures, and imaging. Clinical sources also comment that people in higher-exposure regions may be evaluated based on symptom patterns and exposure history when respiratory illness occurs.

Laboratory methods aim to detect fungal antigens or antibodies and, in some settings, to isolate the organism. Selection of tests varies with site of involvement and clinical context. Imaging such as chest X-ray or CT is used to characterize pulmonary findings, and tissue sampling may be described in sources when localization or characterization of lesions is required.
Learn more about histoplasmosis at Centers for Disease Control and Prevention.

